Abstract
Background: HDT/ASCT can provide a deep hematological response and result in improvement of amyloid related organ dysfunction in a selected group of AL amyloidosis patients (pts.), but is confounded by substantial treatment-related mortality (TRM) compared to multiple myeloma (MM). However, recent trends have shown improved outcomes of HDT/ASCT in experienced US transplant centers with 30-day mortality of 3%. We performed an analysis of the Nationwide Inpatient Sample (NIS) to compare and better delinate the immediate in-hospital complications and mortality in AL amyloidosis and MM pts. post HDT/ASCT.
Methods: The NIS is a large inpatient healthcare database in the US. Unweighted, it contains data from >7 million hospital stays each year and weighted, it estimates >35 million hospitalizations. Full-year data was available for 2008-2013, and this study period was queried to identify patients >18 years of age with a discharge diagnosis of AL amyloidosis and MM after HDT/ASCT conducting a survey weighted domain analysis. Clinical characteristics and in-hospital complications were compared between the two groups using ANOVA test for continuous variables and chi-square tests for categorical variables. Multiple logistic regression was used to compare binary outcomes by AL amyloidosis and MM pts. adjusting for patient characteristics (age, sex, Charlson Co-morbidity Index; CCI).
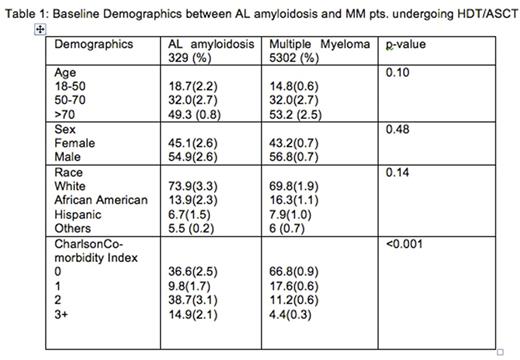
Results: A total of 329 AL amyloidosis pts. were admitted for HDT/ASCT compared to 5302 MM pts. over the 6 year period. The baseline demographics were comparable between the two groups with the exception of CCI (Table 1). Compared to MM, AL amyloidosis pts. were significantly more likely to develop CHF exacerbation (OR 2.69 (95% CI (1.72,4.22); p<0.001); acute renal failure (OR 1.93; 95% CI (1.41,2.66); p<0.001); cardiac arrhythmias (OR 2.19; 95% CI (1.49,3.23); p<0.001); and septic shock (OR 2.14; 95% CI (1.13,4.05); p=0.02); but less likely to develop mucositis (OR 0.56; (95% CI (0.42,0.74); p<0.001) and febrile neutropenia (OR 0.72; (95% CI (0.57,0.91); p=0.005). There was no difference in the use of parenteral nutrition, mechanical ventilation, sepsis and hemodialysis between the groups. Overall, in-hospital mortality in AL amyloidosis pts. was 2.8% compared to 1.3% in MM (p=0.006). On adjusted analysis, there was no difference in in-hospital mortality compared to MM pts. (OR 1.32; 95% CI (0.67, 2.60); p=0.41). The length of stay (LOS) was higher in AL amyloidosis pts. (Mean LOS 20.7 days± 1.01 vs. 17.6 ± 0.52 days; p<0.001) and had higher total hospital charges (mean 185, 000 USD ± 5660 vs. 158,000 ± 8660 p<0.001) compared to MM pts.
Conclusions: The results of our large US-population based study showed that AL amyloidosis pts. undergoing HDT/ASCT had increased rates of cardiac and renal complications, higher LOS and total hospital charges immediate post HDT/ASCT compared to MM cohorts. Despite this, there was no difference in adjusted in-hospital mortality between the two groups, underscoring the ever-improving quality of supportive care, better patient selection and effective drugs in treating these pts. This data may help guide informed consent discussions while providing focus for future studies to reduce treatment-related morbidity in AL amyloidosis pts. receiving HDT/ASCT.
Dhakal: Celgene: Honoraria. Guru Murthy: Janssen: Other: Fellows advisory board. D'Souza: Prothena: Research Funding; Merck: Research Funding; Celgene: Consultancy. Hari: Celgene: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal